Most Number of Cases Osteoid Osteoma Treated By Dr.Ajay Upadhyay
(VISPA0107)
STUDY OF 19 CASES OF OSTEOID OSTEOMA TREATED BY CT GUIDED PER-CUTAENOUS RADIO-FREQUENCY ABLATION OF NIDUS.(january 2010)
Dear Dr. AJAY UPADHYAY
On behalf of the 63rd IRIA 2010 and the Scientific Paper Committee, I would like to express my thanks for your excellent presentation. Your contribution was important to the success of the 63rd IRIA 2010 Conference. It is evident from the comments received that the Scientific Paper Committee and the 63rd IRIA 2010 Board of Directors were not alone in their belief that the Scientific Paper presentation has maintained the tradition of presenting year after year material of high-caliber.
Once again, thank you for the time and effort devoted to the planning and preparation of your presentation. The participation of all radiology professionals, as a whole, continues to make the Scientific paper presentation an effective educational tool that the IRIA has envisioned it to be and has provided best teaching material.
I encourage you to remain active in the Scientific Paper Presentation in the future Radiology Meetings.
Sincerely,
Dr Hemant Patel
Chairman Scientific Committee
63RD IRIA 2010
About Us - Dr. Ajay Upadhyay Radio Frequency Ablation Specialist, Gujarat
Greeting from Dr. Ajay Upadhyay!
I am pioneer to start Radio–frequency-Ablation (Minimal Invasive OPD procedure) in Gujarat in 2007.
Till today (aug 2014) i have performed around 200 RFA of liver and lung and 100 RFA of Osteoid osteoma of bone.
In 100 cases RFA of nidus of Osteoid -Osteoma under CT guidance by Percutaenous route with 100 % clinical success ( femur-57, Tibia -28 ,Spine-4,Scapula-1,Intramedullary-2 others 8) .
This is a FDA approved 1st line of Rx of osteoid osteoma. This is a OPD procedure takes 2-3 hours, under spine/nerve block and precise location of nidus under CT guidance. The patient becomes pain(nidus) free after 24-48 hours and can walk after the procedure.
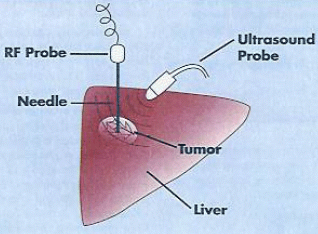
In liver lesion it should be below 5 c.m., less than 3 in no and with normal coagulation parameters with patient require a day admission.
Thanking You,
Yours truly,
Dr. Ajay R Upadhyay.M.D. (Radiology)
(Visiting Interventional Radiologist Gujarat Cancer and Research Institute)
Mediscan, 2nd floor Nandkutir building,B/h Doctor house, C.G.RoadAhmedabad -380006(Gujarat).
(M)- 09825019486
(C)(079)26441832
Email: drajayu@yahoo.com
www.drajayupadhyay.in
What are the benefits vs. risks ?
Benefits
* Radiofrequency ablation can be an effective treatment for primary liver cancer and for cancers that have spread to the liver in select patients whose liver tumors are unsuitable for surgical resection.
* In most studies, more than half of the liver tumors treated by radiofrequency ablation have not recurred. The success rate for completely eliminating small liver tumors is greater than 85 percent.
* Treatment-related serious complications are infrequent and discomfort is minimal.
* Radiofrequency ablation may be used repeatedly to treat recurrent liver tumors.
* The percutaneous method of radiofrequency ablation, in which electrodes are inserted through the skin, is minimally invasive, produces few complications, and does not require hospital admission.
* RFA is a relatively quick procedure and recovery is rapid so that chemotherapy may be resumed almost immediately in patients who need it.
* Radiofrequency ablation is less expensive than other treatment options.
* No surgical incision is needed—only a small nick in the skin that does not have to be stitched closed.
Risks
* Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
* Depending on the site of treatment, radiofrequency ablation may cause brief or, rarely, long-lasting shoulder pain; inflammation of the gallbladder that subsides after a few weeks; damage to the bile ducts resulting in biliary obstruction; or thermal damage to the bowel.
* Roughly one in four patients may develop a "post-ablation syndrome" with flu-like symptoms that appear three to five days after the procedure and usually last about five days. An occasional patient may remain ill for two to three weeks. Acetaminophen or ibuprofen taken by mouth is commonly used to control fever and other symptoms.
* Some cases of bleeding have been reported but it usually stops on its own. If bleeding is severe, an additional procedure or surgery may be needed to control it.
* Organs and tissues near the liver, such as the gallbladder, bile ducts, diaphragm and bowel loops, are at risk of being injured. Although this occurs only 3 to 5 percent of the time, it may require surgical correction. The risk of this complication is related to the location of the liver tumor that is treated.
* Less than one percent of patients may develop a localized infection (abscess) at the site of the tumor ablation three to four weeks after the treatment. A liver abscess will require tube drainage and antibiotics to cure. Patients who have had a surgical procedure in which the liver bile duct has been connected to a loop of bowel are at much greater risk of developing a liver abscess after ablation.
* Women should always inform their physician or x-ray technologist if there is any possibility that they are pregnant.
* This procedure may involve exposure to x-rays. However, radiation risk is not a major concern when compared to the benefits of the procedure.
* Severe pain after RFA is uncommon, but may last a few days and require a narcotic to provide relief.
* Radiofrequency ablation can be an effective treatment for primary liver cancer and for cancers that have spread to the liver in select patients whose liver tumors are unsuitable for surgical resection.
* In most studies, more than half of the liver tumors treated by radiofrequency ablation have not recurred. The success rate for completely eliminating small liver tumors is greater than 85 percent.
* Treatment-related serious complications are infrequent and discomfort is minimal.
* Radiofrequency ablation may be used repeatedly to treat recurrent liver tumors.
* The percutaneous method of radiofrequency ablation, in which electrodes are inserted through the skin, is minimally invasive, produces few complications, and does not require hospital admission.
* RFA is a relatively quick procedure and recovery is rapid so that chemotherapy may be resumed almost immediately in patients who need it.
* Radiofrequency ablation is less expensive than other treatment options.
* No surgical incision is needed—only a small nick in the skin that does not have to be stitched closed.
Risks
* Any procedure where the skin is penetrated carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
* Depending on the site of treatment, radiofrequency ablation may cause brief or, rarely, long-lasting shoulder pain; inflammation of the gallbladder that subsides after a few weeks; damage to the bile ducts resulting in biliary obstruction; or thermal damage to the bowel.
* Roughly one in four patients may develop a "post-ablation syndrome" with flu-like symptoms that appear three to five days after the procedure and usually last about five days. An occasional patient may remain ill for two to three weeks. Acetaminophen or ibuprofen taken by mouth is commonly used to control fever and other symptoms.
* Some cases of bleeding have been reported but it usually stops on its own. If bleeding is severe, an additional procedure or surgery may be needed to control it.
* Organs and tissues near the liver, such as the gallbladder, bile ducts, diaphragm and bowel loops, are at risk of being injured. Although this occurs only 3 to 5 percent of the time, it may require surgical correction. The risk of this complication is related to the location of the liver tumor that is treated.
* Less than one percent of patients may develop a localized infection (abscess) at the site of the tumor ablation three to four weeks after the treatment. A liver abscess will require tube drainage and antibiotics to cure. Patients who have had a surgical procedure in which the liver bile duct has been connected to a loop of bowel are at much greater risk of developing a liver abscess after ablation.
* Women should always inform their physician or x-ray technologist if there is any possibility that they are pregnant.
* This procedure may involve exposure to x-rays. However, radiation risk is not a major concern when compared to the benefits of the procedure.
* Severe pain after RFA is uncommon, but may last a few days and require a narcotic to provide relief.
What is Radiofrequency Ablation of Liver Tumors ?
Radiofrequency ablation, sometimes referred to as RFA, is a minimally invasive treatment for cancer. It is an image-guided technique that heats and destroys cancer cells.
In radiofrequency ablation, imaging techniques such as ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) are used to help guide a needle electrode into a cancerous tumor. High-frequency electrical currents are then passed through the electrode, creating heat that destroys the abnormal cells.
Pictures of Treat liver tumor by Radiofrequency ablation surgery in India.
Radiofrequency ablation needle devices
Radiofrequency ablation needle devices that contain multiple curved, retractable electrodes. The electrodes are kept inside the needle until its tip is positioned within a tumor.
Contact Us - Dr.Ajay Upadhyay, Radio Frequency Ablation (RFA),(Specialist) Ahmedabad
For More Information : -
Dr.Ajay Upadhyay.M.D.
(Consultant Interventional Radiologist)
Visiting Interventional Radiologist -GCRI(Gujarat Cancer and research Institute)
Mediscan, 2nd floor, Nandkutir building,B/h doctor house,
Nr. Parimal underpass, C.G.Road ,Ahmedabad - 380006.Gujarat.India.
Tel :
(079)26441832
(Mo) : 098250 19486
Email: drajayu@yahoo.com
www.drajayupadhyay.in
Labels:
DrAjay Upadhyay,
RFA
RFA Procedure - Radiofrequency Ablation
We first assess the tumor in detail, using CT scans and MRI, which are performed at our centre. However, if these investigations have already been done, we go through them carefully.
If the lesion is suitable for an RFA procedure from the treatment perspective, we assess the technical feasibility.
If the lesion is technically accessible, then a pre-procedure work-up is performed, which consists of a basic health assessment, and the coagulation profile.
If there is no contraindication, the procedure is then performed under deep sedation, with an anesthetist in attendance.
The procedure for an osteoid osteoma takes upto 30-45 minutes. For all other tumors, it may take from 30mins to 2 hours depending on the size of the tumor.
After the procedure, the patient is observed in the post-procedure room, until he/she is fully conscious. Usually within three hours, the patient leaves our centre. The patient is allowed light food four hours after the procedure. The patient will be on oral antibiotic coverage for another 3 days.
With most tumors including osteoid osteomas, the patient can go back to sedentary, non-strenuous work within 24-48 hours.
Follow-up CT scans or MRIs are performed at 48 hours, 30 days and 1 year and are part of the paid-up package.
How is RFA performed?
This technique has many similarities to CT-guided lung biopsy procedures. Throughout the world, lung RFA is commonly performed in a CT scanner suite. Patients undergo this procedure either under moderate sedation with pain relief or under general anesthesia. General anesthesia has the advantage of complete control over patient's breathing pattern and motion that helps to accurately place the RFA electrode within the tumor.
Radio frequency Ablation (RFA) Needle
One study comparing conscious sedation to general anesthesia did not show any major difference in tumor control or procedure related complication rates, however the number of patients in both groups was small . A survey of centers performing RFA for lung tumors indicated that conscious sedation is used more commonly than general anesthesia . During the procedure, tumor cells are destroyed by placing a needle (RFA electrode) within the center of the tumor. The RFA electrodes come in various shapes, length and thickness, depending on the manufacturer . The RFA electrodes are carefully placed into the center of the tumor undergoing ablation using the guidance of images in the CT suite. Multiple CT images are taken to confirm the safe placement of RFA electrodes, and to avoid adjacent vital organs.
Following placement, RFA electrodes are connected to an external RF generator. High-frequency alternating energy is then applied through the RF electrodes. This causes ionic agitation in tumor cells which raises tissue temperature. As the temperature increases above 45-50 degrees centigrade within the tumor, cellular proteins denature and cell structure disintegrates. This results in thermal coagulation in tumor cells, ultimately leading to tumor destruction. The entire RFA procedure session usually takes 3-4 hours or less. Following completion of therapy, RFA probes are withdrawn from the patient. Subsequently, patients are closely observed for any post procedural complications such as lung collapse. Following an uncomplicated RFA procedure, patients are discharged home mostly after overnight observation or rarely the same day.
Lung tissue characteristics may play a role in the effectiveness of RFA. The normal lung tissue surrounding the tumor is relatively resistant to heating due to its high electrical impedance (20, 21). Therefore, the heat energy created by RFA is preferentially deposited in the tumor facilitating higher temperatures. Also, large blood vessels (> 3 mm) near a tumor constantly cool the tissue due to the flowing blood that takes heat away from the area being treated, commonly known as the heat sink effect (14, 20). As a result, tumors in continuity with large blood vessels may be suboptimally treated with RFA. Some electrodes are believed to produce necrosis measuring up to 4-5 cm in diameter. This allows for the treatment of a 3 cm lesion and a 1 cm margin of normal lung. Tumors larger than 3 cm may require multiple electrodes to create overlapping tissue RFA zones.
Radio frequency Ablation (RFA) Needle
One study comparing conscious sedation to general anesthesia did not show any major difference in tumor control or procedure related complication rates, however the number of patients in both groups was small . A survey of centers performing RFA for lung tumors indicated that conscious sedation is used more commonly than general anesthesia . During the procedure, tumor cells are destroyed by placing a needle (RFA electrode) within the center of the tumor. The RFA electrodes come in various shapes, length and thickness, depending on the manufacturer . The RFA electrodes are carefully placed into the center of the tumor undergoing ablation using the guidance of images in the CT suite. Multiple CT images are taken to confirm the safe placement of RFA electrodes, and to avoid adjacent vital organs.
Following placement, RFA electrodes are connected to an external RF generator. High-frequency alternating energy is then applied through the RF electrodes. This causes ionic agitation in tumor cells which raises tissue temperature. As the temperature increases above 45-50 degrees centigrade within the tumor, cellular proteins denature and cell structure disintegrates. This results in thermal coagulation in tumor cells, ultimately leading to tumor destruction. The entire RFA procedure session usually takes 3-4 hours or less. Following completion of therapy, RFA probes are withdrawn from the patient. Subsequently, patients are closely observed for any post procedural complications such as lung collapse. Following an uncomplicated RFA procedure, patients are discharged home mostly after overnight observation or rarely the same day.
Lung tissue characteristics may play a role in the effectiveness of RFA. The normal lung tissue surrounding the tumor is relatively resistant to heating due to its high electrical impedance (20, 21). Therefore, the heat energy created by RFA is preferentially deposited in the tumor facilitating higher temperatures. Also, large blood vessels (> 3 mm) near a tumor constantly cool the tissue due to the flowing blood that takes heat away from the area being treated, commonly known as the heat sink effect (14, 20). As a result, tumors in continuity with large blood vessels may be suboptimally treated with RFA. Some electrodes are believed to produce necrosis measuring up to 4-5 cm in diameter. This allows for the treatment of a 3 cm lesion and a 1 cm margin of normal lung. Tumors larger than 3 cm may require multiple electrodes to create overlapping tissue RFA zones.
Who is suitable for RFA ?
Patients with tumors that are 3 cm or smaller are best suited for RFA treatment. A typical patient undergoing RFA is an adult who cannot undergo lung cancer surgery despite having a tumor that is at an early stage.
Examples of patients who may not be able to undergo surgery include those with poor lung function, other coexisting other diseases, poor general performance status which might deteriorate further following lung surgery, and patients with lung tumors that either do not respond to maximum conventional therapy, including radiation therapy, or recur after treatment. In other words, these patients have tumors that can be potentially removed by surgery, but the presence of other additional diseases in these patients prevent them from undergoing surgery.
Also in this group are patients who cannot afford to lose any more lung tissue. Although few studies report that RFA can be safely performed in tumors close to vital organs such as the heart, generally tumors that are close to the lung hilum (where the airtubes and blood vessels enter the lung) are not amenable to RFA (17, 18).
Examples of patients who may not be able to undergo surgery include those with poor lung function, other coexisting other diseases, poor general performance status which might deteriorate further following lung surgery, and patients with lung tumors that either do not respond to maximum conventional therapy, including radiation therapy, or recur after treatment. In other words, these patients have tumors that can be potentially removed by surgery, but the presence of other additional diseases in these patients prevent them from undergoing surgery.
Also in this group are patients who cannot afford to lose any more lung tissue. Although few studies report that RFA can be safely performed in tumors close to vital organs such as the heart, generally tumors that are close to the lung hilum (where the airtubes and blood vessels enter the lung) are not amenable to RFA (17, 18).
Subscribe to:
Posts (Atom)