Showing posts with label RFA procedure. Show all posts
Showing posts with label RFA procedure. Show all posts
Radiofrequency Ablation of Malignant Liver Tumors - RF Ablation Liver Surgery
What is Radiofrequency Ablation of Liver Tumors?
Radiofrequency ablation, sometimes referred to as RFA, is a minimally invasive treatment for cancer. It is an image-guided technique that heats and destroys cancer cells.
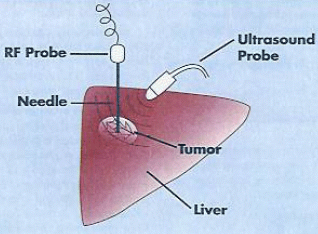
In radiofrequency ablation, imaging techniques such as ultrasound and computed tomography (CT) are used to help guide a needle electrode into a cancerous tumor. High-frequency electrical currents are then passed through the electrode, creating heat that destroys the abnormal cancer cells.
What are some common uses of the procedure?
Radiofrequency ablation is used to treat two types of liver cancer:
- hepatocellular carcinoma,
- Liver metastasis from colon, breast ,endocrine tumor.
In general, radiofrequency ablation is most effective treating tumors that are less than two inches in diameter. It may be used in addition to chemotherapy or radiation therapy or as an alternative to surgical treatment.
Radiofrequency ablation is a viable and effective treatment option if you: are not a good candidate for surgery because your tumor is difficult to reach have other medical conditions that make surgery especially risky would not have enough liver tissue left for the organ to function adequately following the surgical removal of a tumor have liver tumors that have not responded to chemotherapy or that have recurred after being removed surgically you have several small liver tumors that are too spread out to be removed surgically.
Radiofrequency ablation is a viable and effective treatment option if you: are not a good candidate for surgery because your tumor is difficult to reach have other medical conditions that make surgery especially risky would not have enough liver tissue left for the organ to function adequately following the surgical removal of a tumor have liver tumors that have not responded to chemotherapy or that have recurred after being removed surgically you have several small liver tumors that are too spread out to be removed surgically.
How should I prepare?
You should report to your doctor all medications that you are taking, including herbal supplements, and if you have any allergies, especially to anesthesia or to contrast materials (also known as "dye" or "x-ray dye"). Your physician may advise you to stop taking aspirin or a blood thinner for a specified period of time days before your procedure.Prior to your procedure, your blood may be tested to determine how well your kidneys are functioning and whether your blood clots normally.You may be instructed not to eat or drink anything after midnight before your procedure. Your doctor will tell you which medications you may take in the morning.
You may be asked to wear a gown during the procedure.
What does the equipment look like?
In this procedure, computed tomography (CT) and ultrasound imaging, needle electrodes, an electrical generator and grounding pads may be used.The radiofrequency generator produces electrical currents in the range of radiofrequency waves. It is connected by insulated wires to the needle electrodes and to grounding pads that are placed on the patient's back or thigh.
How does the procedure work?
Radiofrequency ablation works by passing electrical currents in the range of radiofrequency waves between the needle electrode and the grounding pads placed on the patient's skin. These currents create heat within the electrode, which when placed within the tumor, heats and destroys the abnormal cells. Because healthy liver tissue is better able to withstand heat, radiofrequency ablation is able to destroy a tumor and only a small rim of normal tissue around the edges of the tumor. At the same time, heat from radiofrequency energy closes small blood vessels and lessens the risk of bleeding. The dead tumor cells are gradually replaced by scar tissue that shrinks over time.
Ultrasound or computed tomography imaging may be used to help the physician guide the needle electrode into the tumor.
What will I experience during and after the procedure?
Devices to monitor your heart rate and blood pressure will be attached to your body.
You will feel a slight pin prick when the needle is inserted into your vein for the intravenous line (IV) and when the local anesthetic is injected.The intravenous (IV) sedative will make you feel relaxed and sleepy. You may or may not remain awake, depending on how deeply you are sedated.
Pain immediately following radiofrequency ablation can be controlled by pain medication given through your IV or by injection. Afterward any mild discomfort you experience can be controlled by oral pain medications. A few patients feel nauseous, but this can also be relieved by medication.You will remain in the recovery room until you are completely awake and ready to return home.You should be able to resume your usual activities within a few days.Only about two percent of patients will still have pain a week following radiofrequency ablation.
What is Radiofrequency Ablation of Liver Tumors ?
Radiofrequency ablation, sometimes referred to as RFA, is a minimally invasive treatment for cancer. It is an image-guided technique that heats and destroys cancer cells.
In radiofrequency ablation, imaging techniques such as ultrasound, computed tomography (CT) or magnetic resonance imaging (MRI) are used to help guide a needle electrode into a cancerous tumor. High-frequency electrical currents are then passed through the electrode, creating heat that destroys the abnormal cells.
Pictures of Treat liver tumor by Radiofrequency ablation surgery in India.
How is RFA performed?
This technique has many similarities to CT-guided lung biopsy procedures. Throughout the world, lung RFA is commonly performed in a CT scanner suite. Patients undergo this procedure either under moderate sedation with pain relief or under general anesthesia. General anesthesia has the advantage of complete control over patient's breathing pattern and motion that helps to accurately place the RFA electrode within the tumor.
Radio frequency Ablation (RFA) Needle
One study comparing conscious sedation to general anesthesia did not show any major difference in tumor control or procedure related complication rates, however the number of patients in both groups was small . A survey of centers performing RFA for lung tumors indicated that conscious sedation is used more commonly than general anesthesia . During the procedure, tumor cells are destroyed by placing a needle (RFA electrode) within the center of the tumor. The RFA electrodes come in various shapes, length and thickness, depending on the manufacturer . The RFA electrodes are carefully placed into the center of the tumor undergoing ablation using the guidance of images in the CT suite. Multiple CT images are taken to confirm the safe placement of RFA electrodes, and to avoid adjacent vital organs.
Following placement, RFA electrodes are connected to an external RF generator. High-frequency alternating energy is then applied through the RF electrodes. This causes ionic agitation in tumor cells which raises tissue temperature. As the temperature increases above 45-50 degrees centigrade within the tumor, cellular proteins denature and cell structure disintegrates. This results in thermal coagulation in tumor cells, ultimately leading to tumor destruction. The entire RFA procedure session usually takes 3-4 hours or less. Following completion of therapy, RFA probes are withdrawn from the patient. Subsequently, patients are closely observed for any post procedural complications such as lung collapse. Following an uncomplicated RFA procedure, patients are discharged home mostly after overnight observation or rarely the same day.
Lung tissue characteristics may play a role in the effectiveness of RFA. The normal lung tissue surrounding the tumor is relatively resistant to heating due to its high electrical impedance (20, 21). Therefore, the heat energy created by RFA is preferentially deposited in the tumor facilitating higher temperatures. Also, large blood vessels (> 3 mm) near a tumor constantly cool the tissue due to the flowing blood that takes heat away from the area being treated, commonly known as the heat sink effect (14, 20). As a result, tumors in continuity with large blood vessels may be suboptimally treated with RFA. Some electrodes are believed to produce necrosis measuring up to 4-5 cm in diameter. This allows for the treatment of a 3 cm lesion and a 1 cm margin of normal lung. Tumors larger than 3 cm may require multiple electrodes to create overlapping tissue RFA zones.
Radio frequency Ablation (RFA) Needle
One study comparing conscious sedation to general anesthesia did not show any major difference in tumor control or procedure related complication rates, however the number of patients in both groups was small . A survey of centers performing RFA for lung tumors indicated that conscious sedation is used more commonly than general anesthesia . During the procedure, tumor cells are destroyed by placing a needle (RFA electrode) within the center of the tumor. The RFA electrodes come in various shapes, length and thickness, depending on the manufacturer . The RFA electrodes are carefully placed into the center of the tumor undergoing ablation using the guidance of images in the CT suite. Multiple CT images are taken to confirm the safe placement of RFA electrodes, and to avoid adjacent vital organs.
Following placement, RFA electrodes are connected to an external RF generator. High-frequency alternating energy is then applied through the RF electrodes. This causes ionic agitation in tumor cells which raises tissue temperature. As the temperature increases above 45-50 degrees centigrade within the tumor, cellular proteins denature and cell structure disintegrates. This results in thermal coagulation in tumor cells, ultimately leading to tumor destruction. The entire RFA procedure session usually takes 3-4 hours or less. Following completion of therapy, RFA probes are withdrawn from the patient. Subsequently, patients are closely observed for any post procedural complications such as lung collapse. Following an uncomplicated RFA procedure, patients are discharged home mostly after overnight observation or rarely the same day.
Lung tissue characteristics may play a role in the effectiveness of RFA. The normal lung tissue surrounding the tumor is relatively resistant to heating due to its high electrical impedance (20, 21). Therefore, the heat energy created by RFA is preferentially deposited in the tumor facilitating higher temperatures. Also, large blood vessels (> 3 mm) near a tumor constantly cool the tissue due to the flowing blood that takes heat away from the area being treated, commonly known as the heat sink effect (14, 20). As a result, tumors in continuity with large blood vessels may be suboptimally treated with RFA. Some electrodes are believed to produce necrosis measuring up to 4-5 cm in diameter. This allows for the treatment of a 3 cm lesion and a 1 cm margin of normal lung. Tumors larger than 3 cm may require multiple electrodes to create overlapping tissue RFA zones.
Subscribe to:
Posts (Atom)